The Future of Telehealth in Australia: From Emergency Measure to Strategic Mainstay
Exploring how Telehealth is changing the landscape of medical practice and improve access to care
When telehealth became widespread in Australia during the pandemic, most people — patients and clinicians alike — viewed it as a temporary solution.
But as the dust settled, a more interesting question emerged: what if remote healthcare wasn’t just a backup plan, but the logical next step in our system’s evolution?
From my experience working across health strategy and digital transformation, I’ve seen that genuine innovation in healthcare doesn’t come from technology alone — it comes from designing systems that meet people where they are. Telehealth, when executed properly, does exactly that.
-
The Shift from Convenience to Core Infrastructure
In the early stages, telehealth was about convenience: replacing travel time with screen time.
Today, it’s far more than that — it’s becoming part of the national health infrastructure.
Australia’s regional and remote communities are now relying on it for continuity of care. For urban patients, it’s solving access bottlenecks that previously left them waiting weeks for basic consults.
This shift mirrors what we see in other industries when a “temporary fix” becomes the new operating model — driven not by cost-cutting, but by efficiency and patient preference.
-
The Data Speaks Clearly
According to the Australian Institute of Health and Welfare, over one-third of GP consultations now include a telehealth component.
More tellingly, patient satisfaction sits above 90% for common conditions managed remotely — including infections, chronic-disease reviews, and prescription renewals.
That level of adoption doesn’t happen by accident. It reflects trust — in the clinicians, in the security frameworks, and in the outcomes.
-
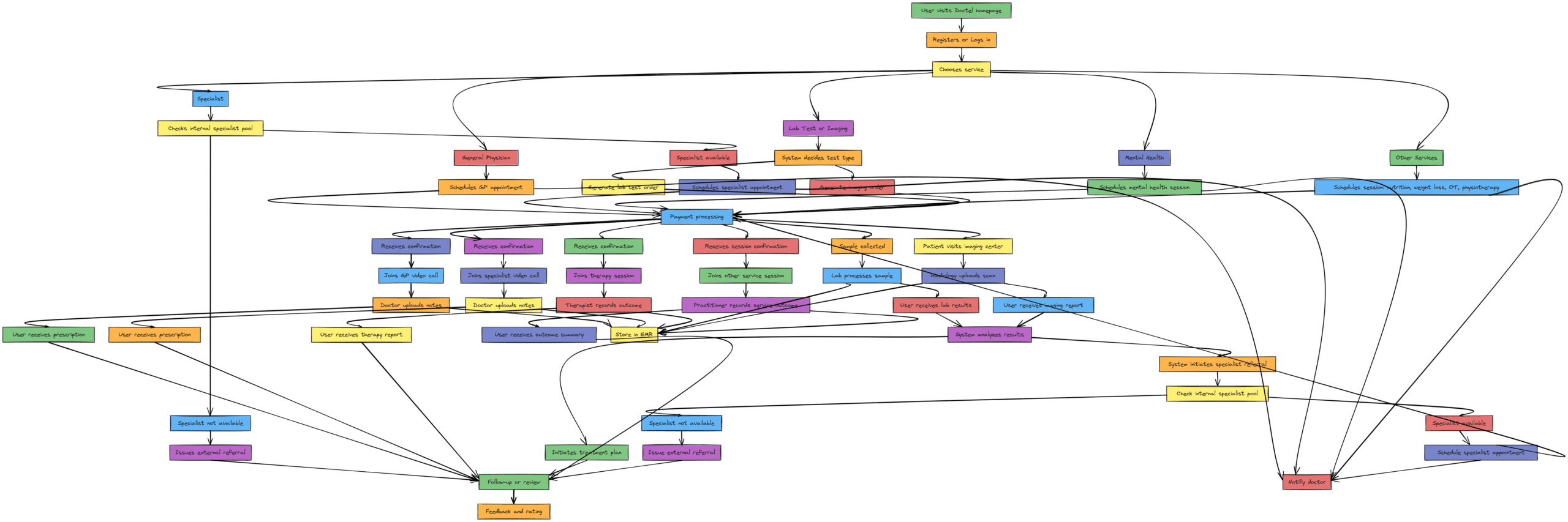
Redefining Clinical Workflows
From a systems-design perspective, telehealth isn’t about moving the clinic online; it’s about rebuilding the consultation model around what actually matters — communication, access, and follow-up.
We now have:
-
Integrated digital records connecting GPs, specialists, and pharmacies
-
e-Prescriptions eliminating physical paperwork
-
Automated follow-ups and reminders improving treatment compliance
The result is less administrative friction and more clinical focus — something every practitioner welcomes.
-
Trust, Regulation, and Patient Safety
A technology is only as valuable as the trust it maintains.
In Australia, telehealth operates under AHPRA and Australian Privacy Principles, meaning every consultation must meet the same legal and clinical standards as an in-person visit.
The platforms that will endure — including ours at DocTel — are those that treat data security not as a compliance checkbox, but as a foundational design principle.
All video sessions, records, and prescriptions remain encrypted and stored within Australian jurisdictions, aligning with OAIC and HIPAA-equivalent requirements.
Patients shouldn’t have to choose between access and privacy — and they no longer have to.
-
The Broader Economic Logic
From a strategic viewpoint, telehealth is reshaping healthcare economics.
Reducing avoidable emergency visits and unnecessary travel improves system efficiency — and, critically, affordability for patients.
It also opens new flexibility for clinicians: hybrid work models, reduced burnout, and broader reach for specialised expertise.
When you align patient experience with clinician sustainability, you get a rare outcome in healthcare — a model that benefits both sides of the equation.
-
Beyond the Consultation: The Preventive Frontier
elehealth’s next growth phase lies in preventive and continuous care.
It’s already transforming how Australians manage their wellbeing:
-
Psychologists and counsellors now deliver long-term support online.
-
Women’s health consultations — from contraception to menopause — are accessible discreetly and quickly.
-
Dietitians and lifestyle specialists monitor progress remotely, making preventive care more consistent.
This shift from episodic to longitudinal care could be the most important structural change in Australian primary health over the next decade.
The Next Five Years
Looking ahead, telehealth will become even more integrated through:
-
My Health Record interoperability
-
AI-assisted triage for early detection and referral
-
Remote monitoring for chronic conditions via wearables and smart devices
As 5G networks expand and healthcare data architecture matures, the distinction between “digital” and “physical” care will dissolve.
Patients will simply choose care — delivered in whatever form best suits their needs.
Conclusion: The Human Layer in a Digital System
Technology has redefined access, but the essence of healthcare remains human.
The clinicians who thrive in this new model are those who bring warmth and clarity to a digital space — the ones who understand that a good consultation is as much about listening as it is about prescribing.
At DocTel, that’s the foundation we build on: using technology to remove friction, not empathy.
Telehealth is no longer an alternative; it’s the evolution of accessible, intelligent, and human-centred care.
Your Health, Your Way — With DocTel
Discover a new era of healthcare with DocTel. Our platform is designed to provide you with personalized, convenient, and compassionate care. Take the first step towards a healthier you by booking a consultation today.