Food Allergies: From Peanut to Alpha-Gal — What You Need to Know
Understanding a Grwoing Global Epidemic
Food allergies have transitioned from an individual medical concern to a significant public-health and economic issue, particularly in countries such as Australia where the prevalence is among the highest in the world. In recent years, clinicians have observed a sustained increase in both the number and severity of food-allergic reactions, affecting children and adults alike. Understanding the immunological mechanisms, diagnostic challenges, and management strategies is no longer the exclusive domain of allergists — it has become essential knowledge for general practitioners, dietitians, and policymakers shaping the future of healthcare delivery.
Understanding Food Allergy: An Immune Error of Recognition
At its core, a food allergy represents a misdirected immune response. The immune system, which is designed to protect against pathogens, mistakenly identifies certain food proteins as threats and mounts an immunoglobulin E (IgE)-mediated reaction. Upon exposure, these IgE antibodies trigger the release of histamine and other inflammatory mediators from mast cells and basophils, resulting in the classic symptoms of allergy — hives, wheezing, gastrointestinal distress, and in severe cases, anaphylaxis.
This immune hypersensitivity must be differentiated from food intolerance, which does not involve the immune system. Intolerances — such as lactose intolerance or caffeine sensitivity — cause discomfort rather than systemic immune activation. The conflation of these two terms has contributed to unnecessary dietary restrictions and public confusion, highlighting the need for accurate education and clinical testing.
Prevalence and the Australian Context
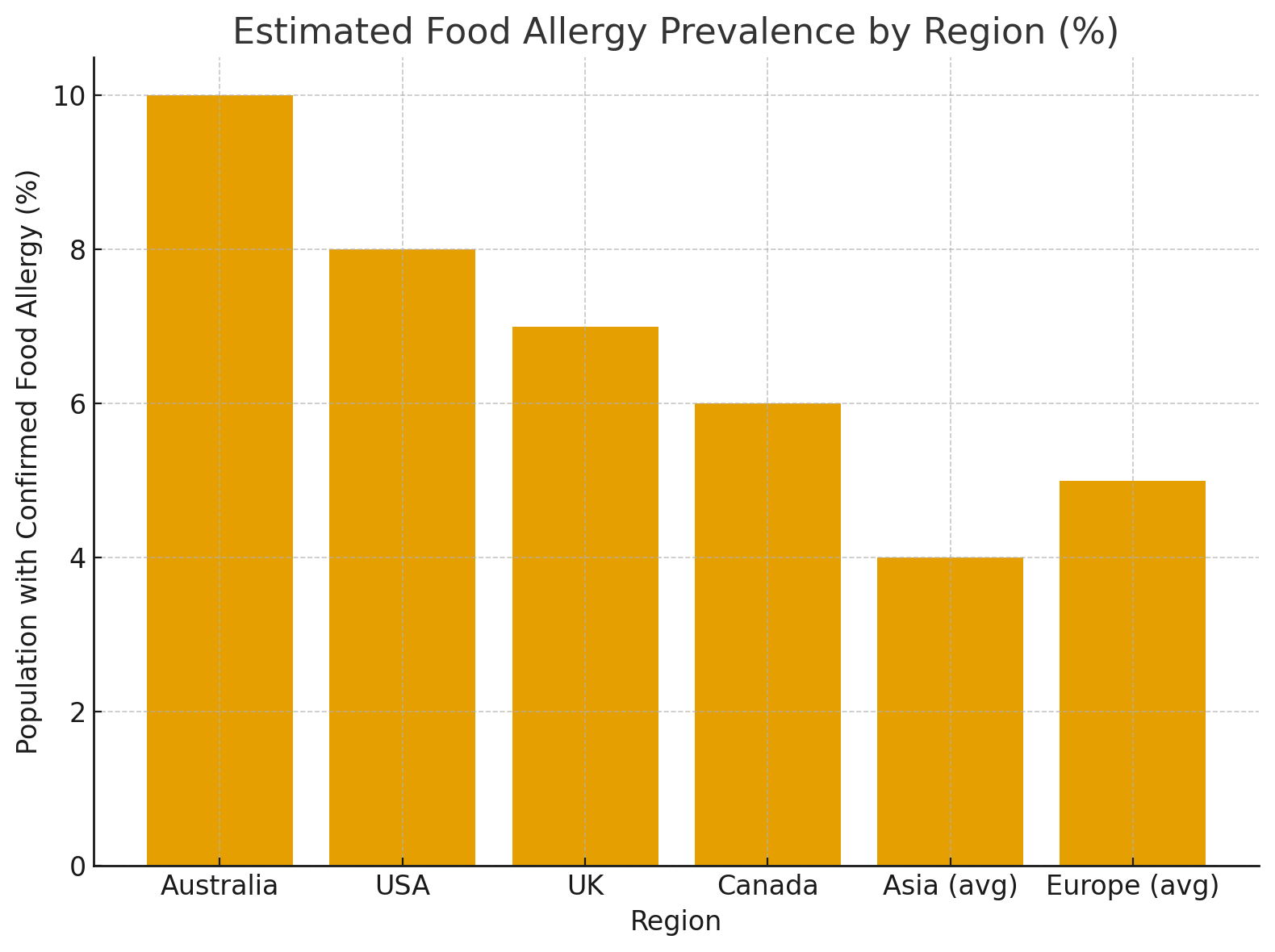
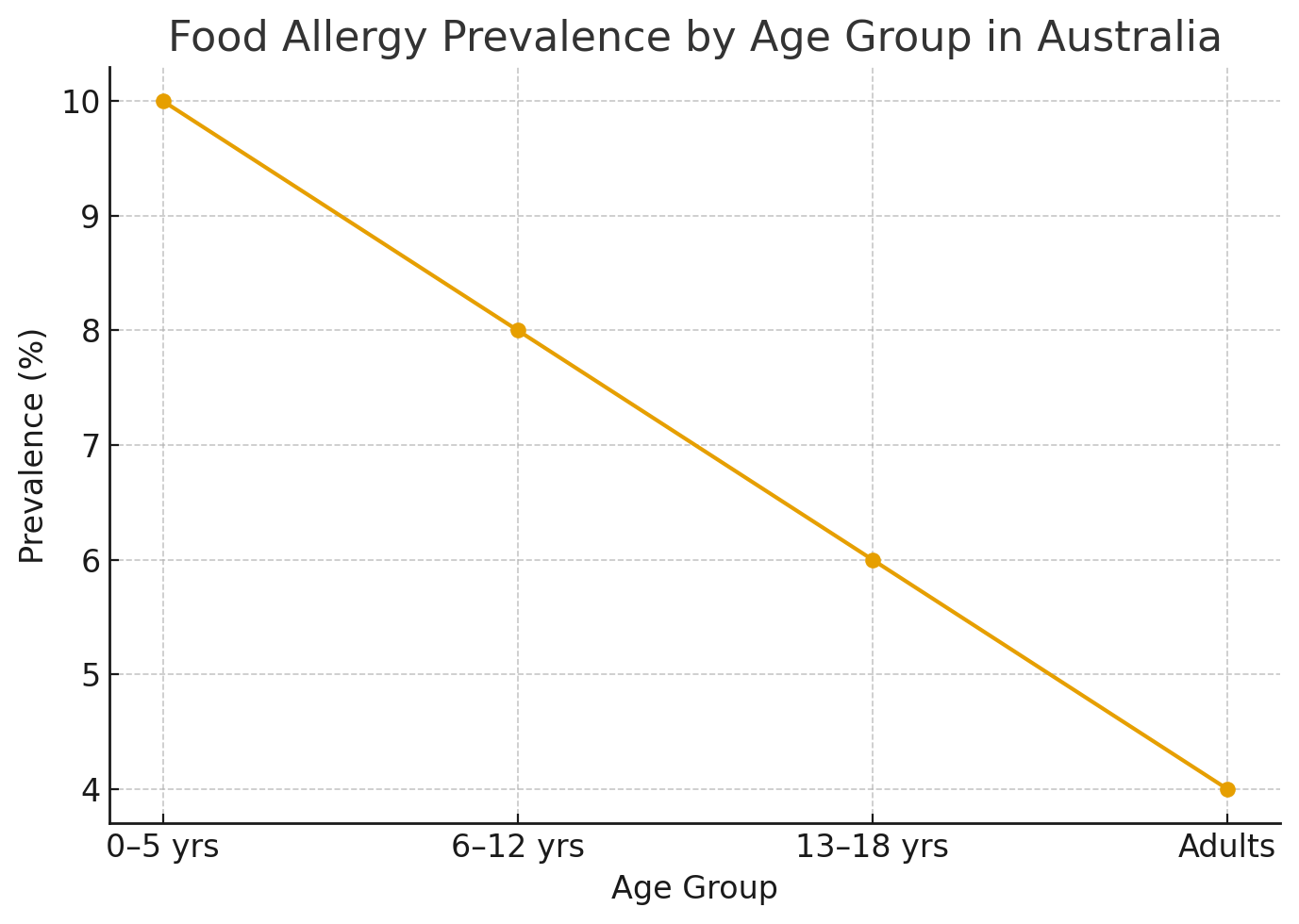
Australia currently records one of the world’s highest rates of food allergy, particularly in children. Studies suggest that up to 10% of infants are affected, with hospital admissions for anaphylaxis increasing steadily over the past two decades. Factors contributing to this rise include genetic predisposition, reduced microbial exposure in early life (“hygiene hypothesis”), altered dietary patterns, and environmental influences such as climate and vitamin D deficiency.
These statistics are not merely clinical curiosities — they have economic and operational implications for telehealth and digital health ecosystems. For providers such as DocTel, understanding allergy risk patterns is integral to designing virtual triage systems, preventive education programs, and specialist referral pathways.
ASCIA 2024; Mayo Clinic 2023; Allen KJ et al., JACI 2013
Common Allergens and Emerging Syndromes
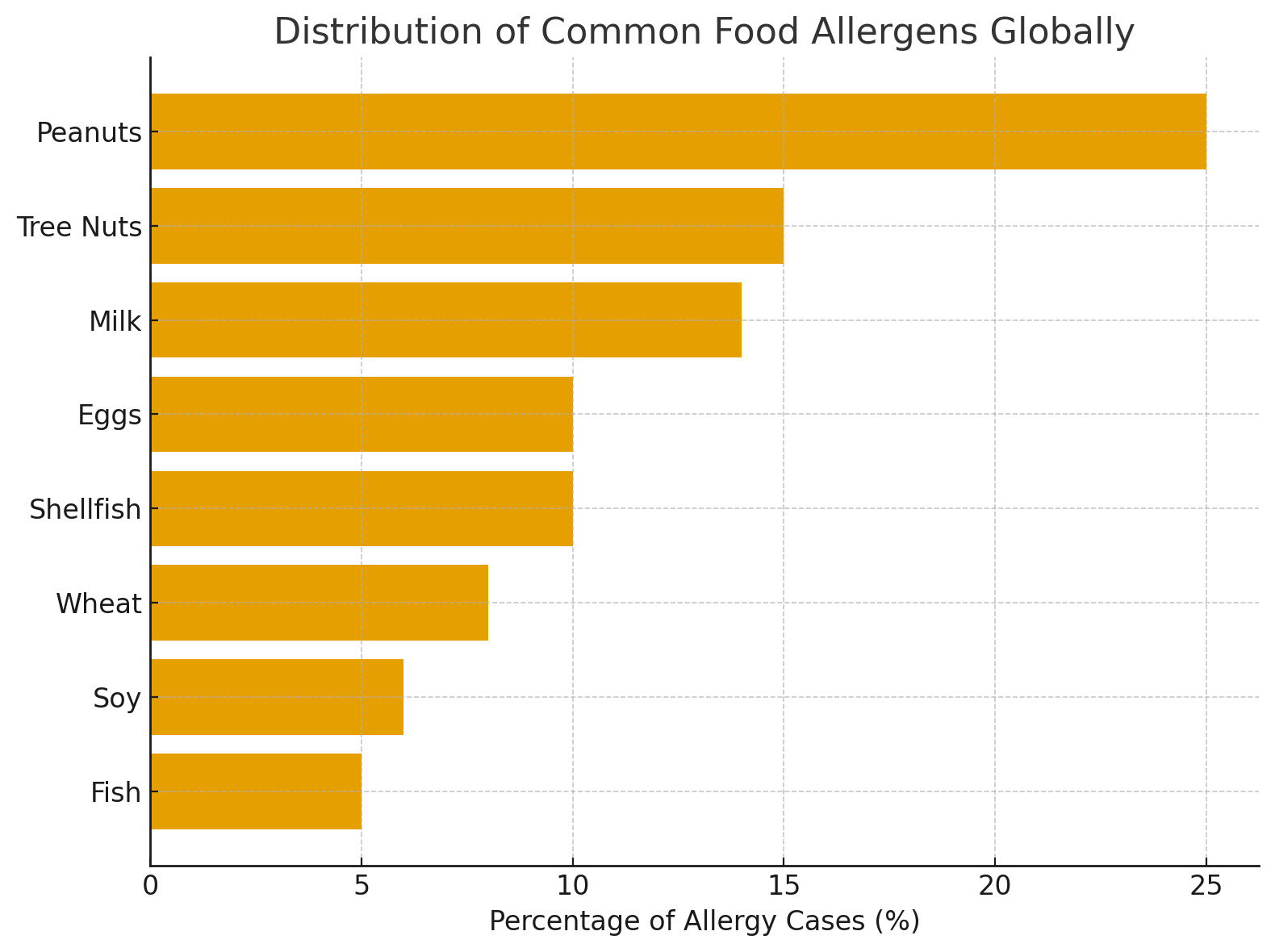
The majority of food allergies stem from a relatively small number of foods — often referred to as the “Big Eight”: peanuts, tree nuts, milk, eggs, wheat, soy, fish, and shellfish. Among these, peanut allergy remains the leading cause of fatal anaphylaxis in Western countries. Even minimal exposure — by ingestion, contact, or inhalation of airborne particles — can be sufficient to trigger severe reactions.
Milk and egg allergies dominate in childhood, with many children eventually outgrowing them by late adolescence. In contrast, allergies to peanuts, tree nuts, and shellfish often persist throughout life. Cross-reactivity between certain proteins can complicate the picture; for example, birch pollen allergy may predispose an individual to oral reactions when eating certain fruits, a phenomenon known as pollen–food allergy syndrome.
In recent years, alpha-gal syndrome has emerged as a novel and intriguing condition. Triggered by the bite of certain tick species (notably the Ixodes holocyclus or paralysis tick in Australia), this delayed allergy to red-meat products can manifest hours after consumption, often during sleep. Unlike typical immediate-type food allergies, alpha-gal reactions are delayed and mediated by IgE antibodies against galactose-α-1,3-galactose, a carbohydrate present in mammalian meat. Awareness of this syndrome remains limited among both clinicians and the public, despite its growing incidence in rural and regional populations.
Mayo Clinic Health System 2024; Gupta RS et al., JACI 2019; Nwaru BI et al., Allergy 2014
Diagnosis: The Science and Its Limitations
Accurate diagnosis is essential but often misunderstood. A patient’s clinical history — timing, reproducibility, and severity of reactions — remains the foundation of assessment. Diagnostic testing, such as skin-prick tests or specific IgE blood assays, can identify sensitisation to particular allergens. However, sensitisation does not always equate to clinical allergy. False positives are common, underscoring the importance of interpretation by an experienced clinician.
The oral food challenge, performed under medical supervision, remains the gold standard for diagnosis. It allows confirmation of true allergy and, in some cases, determination of tolerance thresholds. Nevertheless, this procedure carries inherent risks and is typically reserved for specialist centres. From a systems perspective, the scarcity of allergists in regional Australia presents a gap that telehealth platforms could help bridge — enabling remote consultation and test interpretation within a structured governance framework.
ASCIA 2024; Prescott SL et al., MJA 2017; Allen KJ et al., JACI 2013
Management Strategies: From Avoidance to Immunotherapy
The cornerstone of management remains strict avoidance of the identified allergen. This requires robust patient education, meticulous label reading, and awareness of potential cross-contamination, particularly in restaurants and processed foods. However, avoidance alone does not guarantee safety; accidental exposures remain common.
For patients at risk of anaphylaxis, carrying an epinephrine auto-injector (e.g., EpiPen) is non-negotiable. Epinephrine is the only medication proven to reverse life-threatening allergic reactions by rapidly constricting blood vessels, relaxing airway muscles, and improving cardiac output. Despite this, studies indicate that many individuals either fail to carry their injector consistently or hesitate to use it during emergencies — a gap that must be addressed through continuous patient education.
Dietitians play a pivotal role in ensuring nutritional adequacy, particularly in children or individuals avoiding multiple food groups. Where possible, consultation with an allergy-trained dietitian should form part of the management plan.
The evolving frontier is oral immunotherapy (OIT) — a process of gradually introducing small amounts of the allergen to desensitise the immune system. While early results are promising, OIT is not universally suitable and carries the risk of adverse reactions. Research continues to refine its protocols, with Australian centres contributing to global studies on peanut and multi-food desensitisation.
The Broader Perspective: Prevention, Policy, and Patient Empowerment
Emerging evidence suggests that early introduction of allergenic foods in infancy may reduce the risk of developing allergies — a paradigm shift from past recommendations of delayed exposure. This “early tolerance” approach is supported by studies such as the LEAP trial, though individual risk assessment remains essential.
From a policy standpoint, allergy awareness must extend beyond hospitals into schools, workplaces, and food industries. Mandatory labelling laws, staff training, and public education campaigns have already improved safety, but enforcement and ongoing vigilance are key. The digital health sector, too, can play a transformative role — integrating allergy profiles into patient portals, auto-flagging risks in teleconsultations, and linking with emergency action plans.
Conclusion
Food allergies exemplify the complexity of modern medicine — an interplay between genetics, immunity, environment, and human behaviour. They challenge clinicians to blend precision medicine with public health strategy. For Australia, the high prevalence rate underscores the importance of ongoing research, public education, and innovative models of care.
From a strategic perspective, the intersection of telehealth, dietetics, and allergy management presents an opportunity to deliver more equitable and responsive care — not merely treating allergic reactions, but actively reshaping how allergy-risk patients are supported in everyday life.
References
Mayo Clinic. Food Allergy – Symptoms and Causes.
2024.Mayo Clinic Proceedings. Food Allergy: Pathophysiology and Emerging Therapies. 2023.
Australasian Society of Clinical Immunology and Allergy (ASCIA). Food Allergy Statistics and Guidelines. 2024.
MedlinePlus. Food Allergy Overview. U.S. National Library of Medicine.
Your Health, Your Way — With DocTel
Discover a new era of healthcare with DocTel. Our platform is designed to provide you with personalized, convenient, and compassionate care. Take the first step towards a healthier you by booking a consultation today.